“I was shocked, and I was kind of surprised because she never talked about it, not to me,” Smith said.
The letter, with detailed descriptions of her pain and what nurses go through, shocked her family and inspired them to share her words to help make change for other nurses and health workers.
“I don’t think the general public realizes what these nurses go through,” said Smith, who lives in Patterson Park.
Nationwide, health workers are in the midst of a mental health crisis, the Centers for Disease Control says, caused by the environments they work in and other factors.
More than double the number of health workers reported experiencing harassment at work in 2022 than in 2018, the CDC says, which includes threats, bullying, verbal abuse, or other actions from patients and coworkers.
Of health workers who experienced harassment, 85% also reported feelings of anxiety, 60% reported feelings of depression, and 81% reported feelings of burnout.
‘The law doesn’t protect us, and neither do you.’
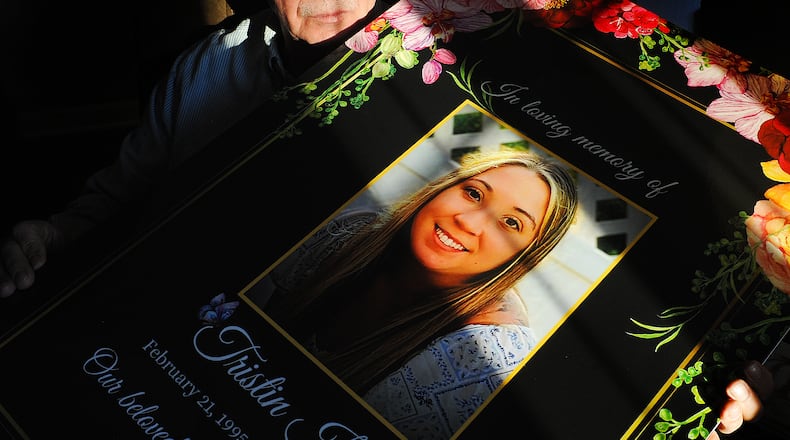
Tristin, a nurse for five years, was an advocate for her patients, as well as her fellow nurses, her family said. If there was a lack of respect or injustice going on, she was going to stand up about it.
“Tristin really did not like injustices,” said Brooke Griffin, one of Tristin’s sisters.
She thought she was entering a career where she would be making a difference, Tristin’s letter says, but she describes feeling like her job took her heart and “slowly crushed the goodness it had.”
Tristin’s letter, which she wrote in March, went viral across the world after her father posted it on his Facebook page. Advocates for nurses say could relate to her pain.
“That letter was shared far and wide among the nursing community, and it definitely resonates with all of us,” said Rick Lucas, president and executive director of the Ohio Nurses Association.
Her working environment was one of “fear and blame,” as well as a place she didn’t feel safe in, Tristin’s letter says.
“You blamed us for things out of our control. You criminally charged my colleagues for things that happened as the direct result of your own actions. The law doesn’t protect us, and neither do you,” Tristin’s letter says.
Tristin wasn’t always getting her breaks and the stress from her job was causing her emotional distress, Smith said. Her letter said she was getting asked “to do more with less.”
Smith tried to encourage his daughter to switch careers, but he speculated she felt saddled by her $26,000 of student loan debt.
“If you’re crying before you go into work, you need a different job. If you’re stressing whenever you get home about it, you need a different job,” Smith said.
Hospitals are understaffed in states where there isn’t a limit on the number of patients per nurses in varying settings, the Ohio Nurses Association says.
This is contributing to poor mental health, they say.
“Suicide and mental health challenges are very real because bedside nurses can’t provide the care patients deserve to the due to the severe understaffing,” Lucas said.
Health workers in crisis
Suicide has been shown to be more common among nurses compared with the general population, according to studies published in the Journal of the American Medical Association.
A more recent study published in September of this year found registered nurses, health technicians, and health care support workers in the U.S. were at increased risk of suicide compared to non–health care workers.
“On behalf of the Greater Dayton Area Hospital Association and our member hospitals, I want to express my sincere sympathy to the Smith family and thank them for speaking so candidly about Tristin’s personal struggles, as well as her experience as a caregiver,” said Sarah Hackenbracht, president and CEO of the Greater Dayton Area Hospital Association. “Too many people in our communities navigate depression alone. We must do better. Sharing Tristin’s story with such raw honesty is a courageous act and an expression of love that shines a light on depression and may help someone else move out of the darkness it creates.”
Hospitals are providing behavioral health support to their employees, such as through employee assistance programs, to provide counseling and other resources, Hackenbracht said.
Family becoming nurse advocates
Tristin’s family is continuing to share her words and her story in the hopes to bring more attention to patient-to-staff ratios in order to help nurses and to prevent other families from experiencing the grief they have.
“One of my goals is, while I’m spreading this word, is to have a state law mandating a safe patient to nurse ratio,” Smith said.
Tristin’s aunt Deb Smith has been mailing copies of Tristin’s letter to health care institutions and colleges, media agencies, and legislators, trying to draw attention to staffing and proposed laws that would create change.
“When I heard the letter, when her dad read it out loud, it was just something that I knew everybody had to hear. It was just a travesty. It broke my heart,” Deb Smith said.
U.S. Sen. Sherrod Brown visited Dayton in April to advocate for pending federal legislation that would set minimum nurse-to-patient staffing standards. The Senate legislation (S. 1113) tracks current California laws and calls for a direct care registered nurse to have limits on their number of patients, depending on the situation.
Credit: AP
Credit: AP
Deb Smith sent hundreds of letters since August, saying she stopped keeping track once she passed 500.
“My hope is finally getting this bill passed,” Deb Smith said about the proposed legislation. “So that other people just don’t feel the darkness that Tristin felt. It had to have been a very scary place, a very lonely place for her to be, and I think our family would really love to see the bill get passed.”
By supporting this legislation, they hope Tristin’s voice is heard, she said.
“We don’t want her death to be in vain,” Deb Smith said.
At the state level, the Ohio Nurses Association has advocated for a proposed bill (H.B. 285) in the Ohio Legislature that would require hospitals to set nurse staffing plans.
“Our hospitals refuse to address this issue,” Lucas said about understaffing. “There are people in charge of our hospitals that are making these decisions that are profit driven and they’re not clinical, and so they’re setting expectations, they’re deciding how many resources we get, and they don’t understand patient care delivery.”
Credit: JIM NOELKER
Credit: JIM NOELKER
Hospitals say they need flexibility when it comes to staffing decisions as multiple factors are taken into consideration, Hackenbracht has previously said.
“[A] singular focus on nurse staffing ratios may divert attention from other critical factors influencing patient safety, such as care coordination, technology integration, and ongoing staff education,” Hackenbracht told this newspaper in September. “Achieving a culture of safety and continuous improvement is essential in health care, which requires a comprehensive approach that goes beyond staffing ratios.”
Violence in ERs
Workplace violence is another stressor nurses are facing, and advocates say more support is needed from hospital administrators.
“I remember the first time I heard about nurses getting hit. I remember that you asked them what they’d done—or didn’t do—to prevent it from happening,” Tristin’s letter says.
Tristin worried about violence impacting her patients and herself, saying she didn’t feel any support.
“I no longer feel like you care about me or the people you say you serve. I sit at my front desk just waiting for someone to walk in off the street and shoot my patients and me; you do not care about keeping us protected,” Tristin’s letter says.
Violence in emergency departments has been a growing issue for the past decade. The incidence rate for workplace violence to health care workers has increased since 2011, according to the U.S. Bureau of Labor Statistics. The health care and social service industries experience the highest rates of injuries caused by workplace violence and are five times as likely to suffer a workplace violence injury than workers overall.
“Hospitals throughout the Dayton region continue to navigate their shared mission of serving their communities at a time when the increased incivility towards caregivers has escalated. Violence in hospitals and health systems has increased since the onset of the COVID-19 pandemic along with acts of violence against health care workers throughout the care continuum,” Hackenbracht said.
Hospitals are developing their own police forces, as well as tracking patients who have a history of violence, Hackenbracht said. Patient code of conduct policies are also being developed to as many organizations move to “no” or “zero” tolerance policies when it comes to violence, she said.
“Legislatively, hospitals are working to pass the bipartisan, bicameral Safety from Violence for Healthcare Employees (SAVE) Act that would give healthcare workers the same legal protections against assault and intimidation that flight crews and airport workers have under federal law,” Hackenbracht said.
Policies that address workplace violence and support health workers are needed, and hospitals need to back their employees, Lucas said. While he is currently part of a union where he works now, he said he used to see situations where workers were threatened with HIPAA privacy violations if they called the police because they were assaulted.
“That does happen where health care workers are threatened and coerced by hospital administration not to call the authorities, not to press charges, not to seek help,” Lucas said.
Another thing hospitals can do is preserve nurse staffing committees and give them meaningful representation in establishing those safe staffing levels, Lucas said.
“Regardless of what’s happening, it’s never okay to put your hands on somebody else...but we have patients coming in that are in pain, that are afraid, their loved ones are with them, and they see them in pain, and they’re afraid for them, and so sometimes they’re upset because we’re not able to meet those demands,” Lucas said.
By not having the resources nurses and staff need, it causes harm and puts pressure on the system, he said.
“The executives aren’t there facing the consequences, but it puts a lot of pressure on the system, it puts a lot of pressure on people in crisis, and so by not having the resources that we need, they’re putting us all in a really bad place,” Lucas said.
‘A new normal’
Tristin’s family is bracing for the first Thanksgiving without her, whom her family said was always around, ready to spend to time with them. Tristin was an animal lover, often visiting her father’s house, who lived nearby, with her blue pit bull.
“It’s going to be difficult because one of our family members is not (here),” Smith said.
“She was the one who was always around, too, like you could always guarantee that Tristin would be around the holidays, so we have to create a new normal,” Griffin said.
Tristin would love these efforts to use her letter to help other nurses, her family said.
“She’s always showing up (for others)… She would be so happy,” Griffin said.
Where to go for help
A national hotline that is available for use is the 9-8-8 Suicide and Crisis line, where crisis resources are provided to individuals by a trained crisis counselor.
The Mental Health Recovery Board, which serves Warren and Clinton counties, offers a 24/7 Crisis Hotline at 877-695-6333 or Crisis Text Line “4Hope” 741741.
The Butler County Mental Health and Addiction Recovery Services Board’s crisis lines are 1-844-4CRISIS or 1-844-427-4747.
In Montgomery County, the Crisis Call Center can be reached at 833-580-CALL (2255), and it is operated by RI International, a mental and behavioral health services non-profit. Since it started taking calls in January 2022, it has received more than 18,000, with 89% of the calls being resolved over the phone. The average time on the call is 14 minutes, and 0.63% of the calls get transferred to 9-1-1.
In Clark County, the crisis hotline is 937-399-9500, and in Greene County, the crisis hotline is 937-376-8701.
The Tri-County Board of Recovery and Mental Health Services, which serves Darke, Miami, and Shelby counties, offers a 24-hour crisis hotline at 800-351-7347.
About the Author