Mercy Health said Anthem, referencing Anthem’s parent company, Elevance Health, has stopped negotiations, but Anthem disputes that statement.
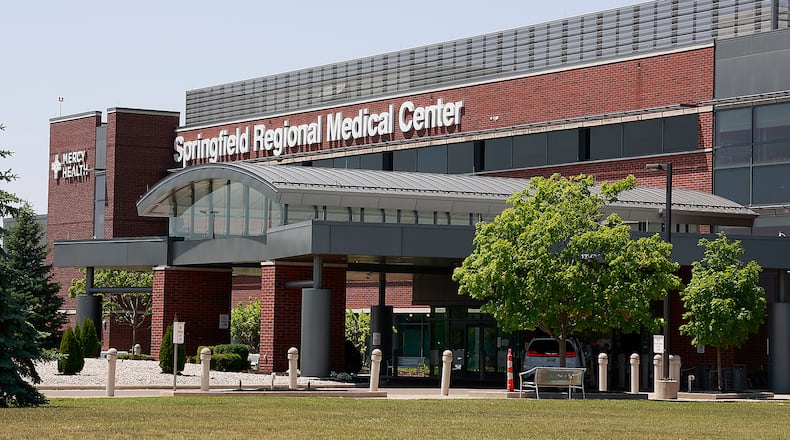
“Mercy Health has been in negotiations with Anthem (aka Elevance Health) for nine months, and we have been unable to reach an agreement on rates. In fact, Anthem recently rescinded its most recent offer and discontinued negotiations. This means that nearly 50,000 Ohioans (including 3,624 in the Springfield market) may lose their Medicaid insurance coverage with Mercy Health beginning July 1 and may be forced by Anthem to leave doctors they know and trust,” said Jennifer Robinson, public relations and communications manager for Bon Secours Mercy Health.
Anthem began serving Ohio Medicaid members on Feb. 1, but they have served Medicaid members in other states prior to then.
Anthem and Mercy Health have recently-signed contracts in place for all lines of business until Jan. 1, 2025, said Jeff Blunt, communications director for Anthem Blue Cross and Blue Shield in Ohio. Medicaid, though, allows hospitals to terminate contracts with 60 days notice.
“We remain firmly at the negotiating table, and we continue to advocate for solutions that do not include the termination of contracts for our most vulnerable populations. We are committed to reaching a resolution that avoids care disruption for our members. It’s important to remember that Bon Secours Mercy Health choose to cut off services mid-contract for our Medicaid members if we do not agree to dramatic price increases for those on our individual and employer-based plans,” Blunt said.
Mercy Health also notified Anthem it will no longer accept Anthem Medicare Advantage members on Oct. 1 unless Anthem agrees to “higher costs for our employer-based and individual plan members,” Blunt said.
Higher rates are needed to keep up with labor and supply costs, Mercy Health said.
“Health care organizations across the nation, including Mercy Health, have been experiencing significant inflationary, labor and supply cost challenges,” Robinson said. “Our labor costs have increased 9.6% while supply chain shortages and inflation have increased our operating expenses and overall cost of care by 6.8% from 2021 to 2022. It is critical that our patients have access to the care they need when they need it, and reimbursement to cover our costs is an important part of that equation.”
Mercy Health also referenced reports of quarterly earnings for Anthem’s parent company, Elevance Health, of $2.8 billion, an increase of 16.6% year-over-year, when saying Anthem owes Mercy Health more than $100 million in late and unpaid claims.
Mercy Health has declined to provide additional information to substantiate their late and unpaid claims statement, Blunt said.
“In the normal course of business, there is a lag in claims submission and payment as we perform our responsibility to assure claims are submitted and paid accurately. This is a critical role all health insurers play in the system,” Blunt said. Over the last 12 months, 92% of Anthem claims are being processed within 14 days, and 98% within 30 days, he said.
When asked about what rates are being discussed, Mercy Health declined to answer and Anthem said it could not go into specifics.
“Due to the confidential nature of the negotiations, I can’t give you specific numbers. But can tell you that the requested increases are more than double the current hospital inflation rate,” Blunt said.
Mercy Health also isn’t asking for increased payments for Anthem Medicaid, Blunt said.
“Mercy Health is using Ohio Medicaid members, a population particularly vulnerable to health care disruption, as a tactic to force higher costs onto commercial plan members and their employers,” Blunt said.
Anthem employer-based and individual health plan members are currently not being impacted by these negotiations.
About the Author