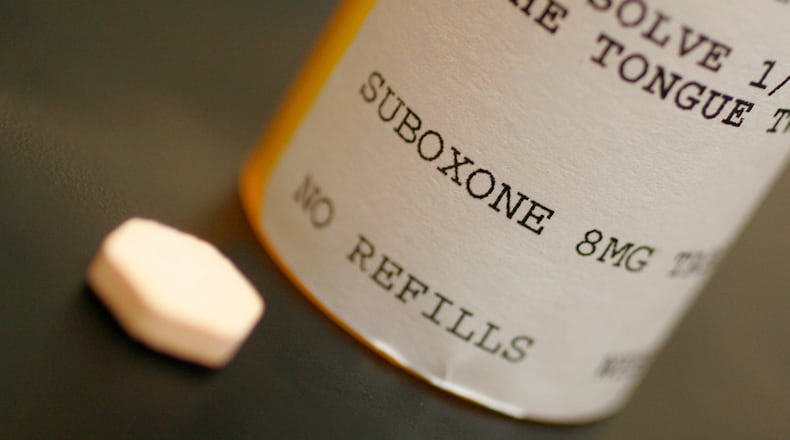
The state already requires patients receiving Suboxone to get counseling. The proposed rules specify what type of counseling or therapy qualifies.
Several doctors have raised issues with the requirement to get counseling, saying it isn’t medically necessary and limits the number of doctors offering MAT and number of patients getting help.
RELATED: Millions of tax dollars pay for new drug treatment -- is it working?
“There are a lot of barriers that we’re putting in the face of treatment,” said Dr. Jeanette Moleski, a board certified addiction and family medicine doctor in Portage County near Cleveland. She wrote to the board about the rule changes saying, “What I am afraid more rules will do is keep good physicians and other providers from even considering treating people with addiction.”
Others in the treatment community say giving someone Suboxone without treating the underlying behavioral problems will not lead to long-term recovery.
“Addiction is a disease … It’s also fundamentally a lack of skills,” said Marcia Weber, manager of program development and quality assurance at Cornerstone Project treatment center in Dayton.
Is counseling necessary?
The Ohio Society of Addiction Medicine has objected to the counseling requirement, citing a 2018 Substance Abuse and Mental Health Services Administration document called Treatment Improvement Protocol 63.
“Four randomized trials found no extra benefit to adding adjunctive counseling to well-conducted medical management visits delivered by the buprenorphine prescriber,” it says.
Gregory Boehm, the Ohio society’s president, wrote the group agrees. “Counseling does not improve outcomes,” he said.
That document also makes references to the benefits of counseling.
“Counseling helps people with (opioid use disorder) and other substance use disorders change how they think, cope, react, and acquire the skills and confidence necessary for recovery,” the document says.
Behavioral health experts say treatment drugs like Suboxone help patients avoid overdose and death by blocking their craving for opioids. But they believe it’s the psychosocial treatment that changes behaviors and leads to long-term recovery.
“Does it work for people to not kill them? Absolutely,” said Kyle Zink, assistant clinical supervisor of Woodhaven Residential Treatment Center in Dayton. “Does it change them? I don’t know.”
The Path Forward: Addiction in Dayton
- » Millions of tax dollars pay for new drug treatment -- is it working?
- » This local drug court cut rate of new felonies by more than half
- » Dayton getting national credit for battling opioid crisis
- » Vets twice as likely to fatally OD -- what the Dayton VA is doing about it
- » Foster care system struggles to keep pace with opioid epidemic
- » New challenge for recovering addicts: Finding a job
- » Can Dayton go from 'overdose capital' to a model for recovery?
- » Mother of 7 rebuilding family after addiction
- » A day with Dayton's overdose response team
Woodhaven’s program is abstinence based, but it doesn’t turn patients on medication-assisted treatment away. The center has had clients who have tried Suboxone and failed to stay sober — sometimes moving to methamphetamine instead, Zink said.
Others want to get off Suboxone as they move into long-term recovery, he said, because they still feel anxious about needing a substance to get through the day.
While counseling can help, some doctors say they fear a requirement will cause some patients to forgo treatment. Moleski gave the example of Type II diabetes.
“It is almost 100 percent preventable with diet and exercise, yet we don’t take their medication away if they don’t go to diabetic classes,” she said.
Many of those in addiction will take the path of least resistance if given a choice, Weber said. But if forced to attend counseling, they will do it begrudgingly.
“The goal is to allow them to be out of distress enough to learn,” she said.
More rules needed?
Cornerstone Managing Partner Mike Ward wants to see the medical board enact more rules for MAT.
He’s concerned about some doctors he sees in Dayton who are operating cash-only clinics, giving out Suboxone with no other services or referrals to further treatment. For about $200 a client can get a 90-day prescription, which he said they can turn around and sell on the street for $2,000.
RELATED: Addiction doctor: Drug dealers are profiting off Medicaid
And while they paid cash to the doctor for the visit, they may have used Medicaid to fill the prescription, meaning tax money is funding street drug trade, Cornerstone staff members said.
“Until the Ohio Medical Board can reign these doctors in, we’re going to see the same results,” Ward said, meaning more overdoses and deaths from opioids.
Montgomery County saw a reduction in overdose deaths from 566 in 2017 to 292 in 2018. More access to treatment, including more doctors able to prescribe Suboxone in their practices, has been credited with helping to move the needle on opioid deaths.
Moleski is also concerned about bad medicine.
“I understand the State Medical Board of Ohio’s desire to put these doctors out of business,” she said. “The issue is bad doctors are not going to become good doctors because you give them more rules.”
Changes moving to review committee
The state medical board made several changes to the proposed rules after the comment period but kept the requirement for counseling. The changes have been submitted to the Joint Committee on Agency Rule Review and are expected to be on the committee’s agenda for review on March 4.
One of the changes made based on the comments covers a patient who refuses to attend counseling. Originally the alternative was participation in a 12-step program. Moleski pointed out in her letter to the board that 12-step is a faith-based program and it would be unconstitutional to require attendance.
The wording now says 12-step or other self-help recovery program.
RELATED: No Carfentanil spike locally, but OD deaths are up
Moleski still has questions about how the rules will work in practice. For example, she asked if a patient stays on Suboxone for years, do they need to be in counseling or therapy for years?
“It doesn’t say how long that needs to continue. It’s very unclear,” she said.
Experts on both sides of the argument say the best plan is an individualized approach.
“We have people that will do very well without the counseling,” Moleski said. “There are people that absolutely have to go to counseling … I really wish this could be more individualized.”
ABOUT THE PATH FORWARD
We have formed a team to dig into the most pressing issues facing the Miami Valley. The Path Forward project, with your help and that of a 16-member community advisory board, seeks solutions to issues readers told us they were most concerned about.Follow the project on our Facebook pages and at DaytonDailyNews/PathForward, and share your ideas.
About the Author