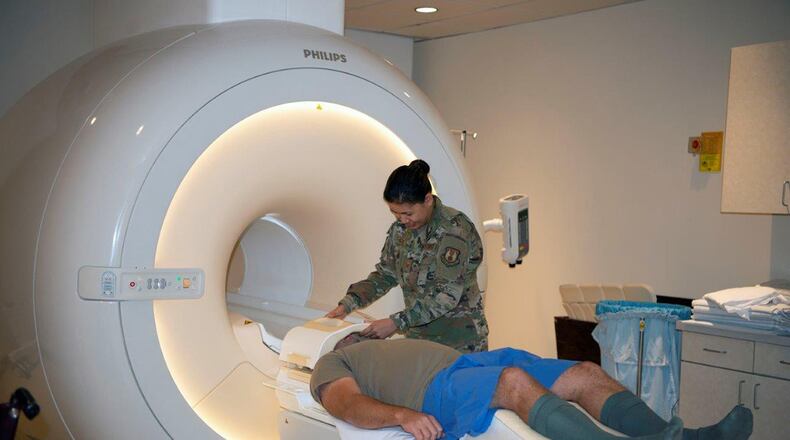
Tech. Sgt. Mariecrist Shuty, 88th MDG MRI specialist, said that whether they are deployed or at home, they want to make sure they perform proper exams to help ensure providers are able to give patients the right diagnoses.
There are four Airmen and two contractors who work in the 88th MDG’s Diagnostic Imaging Flight’s MRI section from 6 a.m. to 8 p.m., Monday through Friday. They scan an average of 20 patients a day, which is about 400 patients per month or more than 5,000 patients a year.
They operate an MRI scanner that has 10 MRI coils and uses as many as 12 cameras. The coils create a magnetic field or detect a changing magnetic field. They provide the magnetic field to align the atoms around the area being scanned. Those atoms are then excited by radio waves, and the cameras capture the internal images. The images taken are sent to a computer for interpretation using MRI software.
Each area of the Diagnostic Imaging Flight has its own advantages for assisting doctors in making patient diagnoses. While MRI scans can be used for any part of the body, doctors may also order scans when looking into soft tissue or nervous system injuries or diseases.
“MRI is more detailed but also very motion sensitive,” said Staff Sgt. Jason Stromvall, an MRI specialist, who is also trained in computed tomography, in comparison to the other areas of diagnostic imaging.
He added that the scanner’s sensitivity to motion is also a disadvantage in some cases, mainly for patients who are unable to hold still like children or people who are claustrophobic and might become anxious during the scan.
“To add to that, [in] MRI, we don’t use radiation,” said Shuty, who is also trained in interventional radiology and mammography.
Instead, MRI scanners use non-ionizing radiation.
Stromvall agreed and said when being scanned, heat can be created and cause the patient’s body temperature to rise, but, unlike X-ray, it doesn’t affect the patient’s cells and cause them to mutate.
When performing scans, MRI specialists are not only concerned with taking proper precautions and performing procedures correctly for the diagnosis purposes, but also for patient safety.
“An extremely important part is making sure they’re safe to enter the MRI environment because it’s a very strong magnet,” said Stromvall.
He added that some of the things they need to be aware of concerning their patients are whether they have a pacemaker, metal injuries to the eye, neurostimulator implants or a history of any kind of brain procedures. Another thing they have to take into consideration is whether a patient is using a medicine infusion pump because the MRI scanner can affect whether it properly dispenses the medication.
Airmen with the 4R0X1 Air Force specialty code complete their traditional training as diagnostic imaging specialists, which prepares them for taking and assisting with X-rays, but they must go through additional training before they are able to work in MRI. As well as completing the training, like their civilian counterparts, WPAFB Airmen are also eligible to be certified by the American Registry of Radiologic Technologists.
Stromvall said that like a lot of the major MTFs in the Air Force, they have knowledge and experience. “They also have multiple credentialing measures in place from the American Registry of Radiologic Technologists, an organization that governs us and certifies us,” Stromvall said.
Shuty and Stromvall both agreed patients should trust them because they enjoy the work they do and enjoy helping their patients.
About the Author